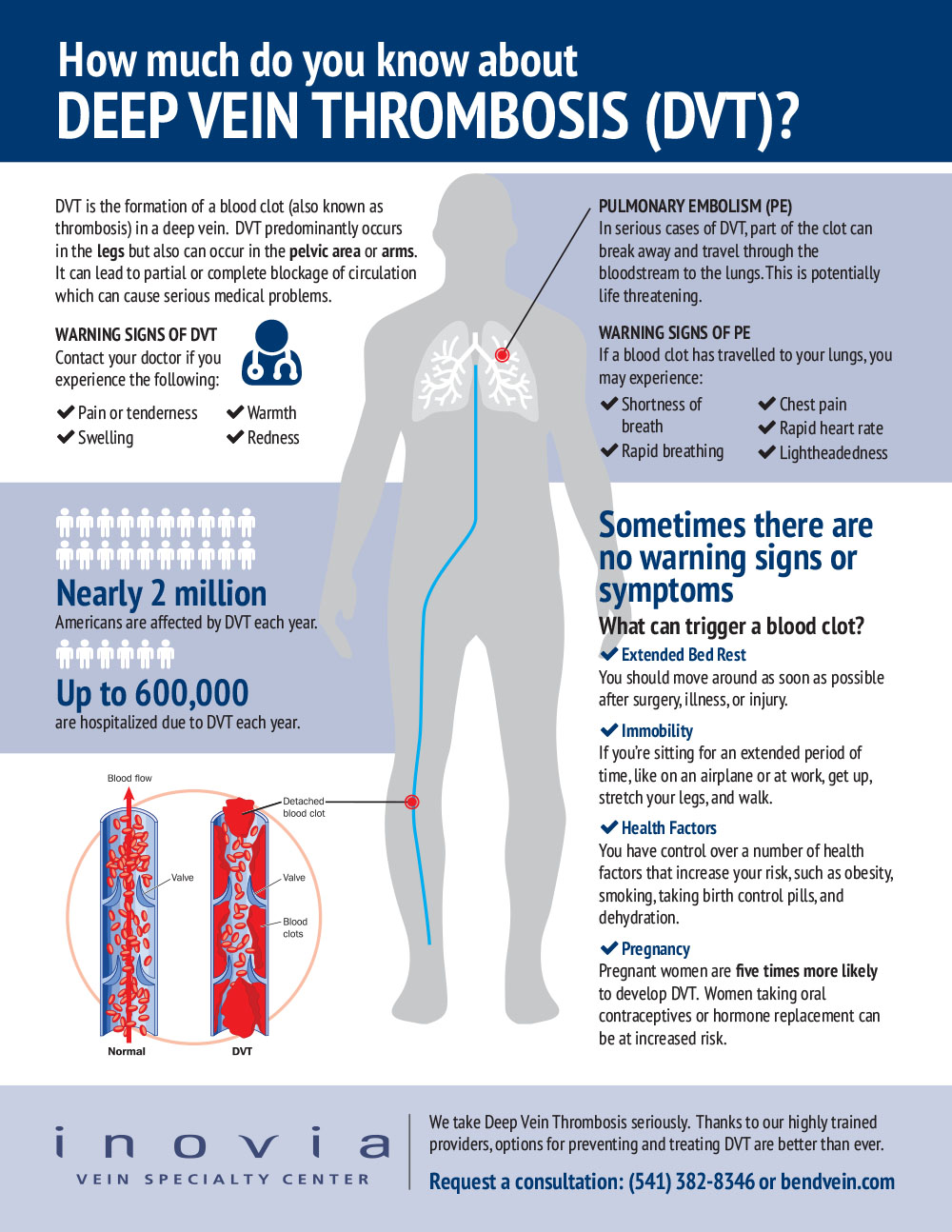
Deep Vein Thrombosis (DVT) is a blood clot most commonly found in the deep veins of the legs, pelvis or arms. When a clot forms in a deep vein, blood flow is re-routed and pressure builds. This can lead to swelling, pain, and redness in the leg since the blood flow from the leg to the heart is being blocked.
Short term risks of a DVT?
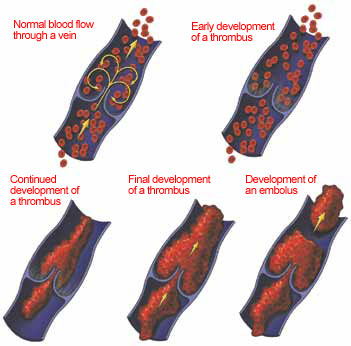
One of the most dangerous complications of a DVT is that the clot can break free in the vein and travel to the lungs and heart. This is known as a pulmonary embolism, or what health care workers call a PE for short.
Almost everyone has heard that a pulmonary embolus can be a fatal complication of a DVT, and thus simply hearing that a DVT is a possibility strikes fear into most people.
Not all PEs are fatal. What determines the seriousness of a PE is the size of the clot and the numbers of clots that break off and go to the lung blocking oxygen supply or which block blood flow in the heart, causing heart failure.
Generally, the larger the vein with the DVT, the more danger there will be a fatal or near fatal PE. Thus when you are discovered to have a DVT, the healthcare providers will often assess the size of the DVT by determining the size of the vein with the clot. Usually, the closer the vein is to the heart and lung the bigger the vein, and thus the bigger the clot if a DVT is present. This is to say that an isolated clot in the very small veins by the ankle is not as serious as a large clot extending from the leg though the pelvis to the vena cava.
Occasionally, one or more pulmonary embolus is found when no DVT is noted in the legs. This can occur when the entire clot has broken off and traveled to the lung, or if the clot is coming from a source other than the legs, such as the pelvic veins or the arm veins. Even a small DVT that breaks loose can sometimes be fatal.
A rare condition, known as a paradoxical embolus, occurs when a small clot passes through a small hole that nearly 20% of all individuals have in their heart (the foramen ovale), which allows the clog to bypass the lungs and travel to the brain, causing a stroke.
The treatment for a PE is very similar to the treatment for a DVT, with the exception of a massive PE that occasionally require a hospital endovascular procedures to break down and remove the clot.
Long-term risks of DVT’s?
While most patients are aware of and fear the potential short term complications of a DVT, few are aware of and understand that blood clots in the veins of the legs can cause long-term problems.
Most of the clot that occludes venous segments recanalizes (disolves away) over the first 6 to 12 months after an episode of acute DVT, leading to chronic changes in the structure of the vein, and in many cases, failure of the veins to function as conduits taking blood back up to the heart. This occurs because clots in the veins can damage the valves of the vein that help propel blood upward against gravity, and prevent pooling of blood in the legs.
The damage commonly leads to a reversal of flow in the veins, and high pressures in the lower leg. This high pressure in the veins can contribute to the development of chronic pain and swelling in the legs. Worse yet, these changes in the blood flow dynamics of the leg veins after a DVT actually increase the chance of developing another blood clot in the veins in the future.
In addition, blood clots can lead to chronic pain and swelling in the leg, a condition called post-thrombotic syndrome (PTS). Post-thrombotic syndrome varies from mild swelling to incapacitating swelling with pain and ulceration. This occurs in up to 60% of patients with a history of DVT, and about 10% of these people will have skin break down in the lower part of the leg, called a venous stasis ulcer.
Signs and Symptoms of a DVT
- Leg swelling
- Ache
- Pain
- Redness

How do compression stockings help after the diagnosis of a DVT?
Compression stockings are important in the treatment of DVT’s, especially when swelling is present. Ideally, a person with a new diagnosis of a DVT should wear graduated compression stocking shortly after the time of diagnosis of a DVT. This can help how the leg feels acutely by minimizing swelling, but it may also impact the long term health of the leg.
It is important that people have true graduated compression stockings, which apply 20 – 30 mmHg compression starting at the ankle, as opposed to anti-embolic stockings (sometimes referred to as TED hose) which, depending on the manufacturer, deliver in the range of 8 – 18 mmHg.
When a patient is up and walking, the pressure generated in the veins after a DVT can be significantly higher than when they are laying down. This explains why the primary difference between anti-embolic stockings and graduated compression stockings is that anti-embolic are designed for a bed-ridden patient (when the compressive pressure requirements are lower) and graduated compression stockings are for patients who are ambulatory and require a higher compression level. The increased pressure applied to the leg allows for better control of symptoms, especially swelling, ache and tiredness.
The stocking should be put on in the morning and can be taken off in the evening. It is important to remember that the elastic in the compression stocking wears out over time, and therefore new stockings should be purchased every 4-6 months or so. Proper care can extend the life of the stockings.
How can I prevent a DVT?
Deep vein thrombosis is often a preventable disease. People undergoing surgery and in the hospital are at risk for developing blood clots, and your health care provider will help you to prevent DVT’s in these situations. If you are not in the hospital, you still can develop blood clots.
Smoking cessation will minimize your risk of DVT’s as well as many other diseases. Obesity has been shown to increase the chance of blood clots. Weight loss and exercise can decrease this risk and is good for your overall health.
Travelers are also at risk of DVT’s. In particular, if you are traveling for a long period of time (over 4 hours), you are at increased risk of having a blood clot. You can decrease this risk by getting up and walking if you are on a plane, or making frequent stops and moving around if you are on a long car drive. Graduated compression stockings worn while traveling have also been shown to decrease the rate of blood clots in the legs.
Unfortunately, if you have had a prior blood clot, you are at increased risk of developing another blood clot. It is important that you are familiar with the DVT symptoms so that if you develop a new blood clot you can seek immediate medical treatment.